65 year old female
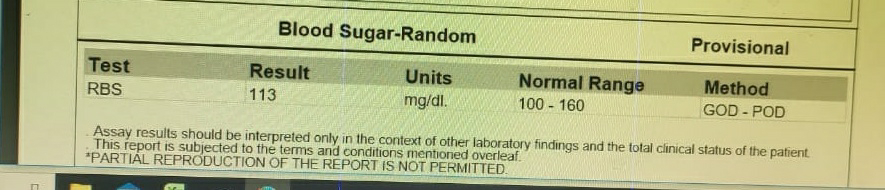
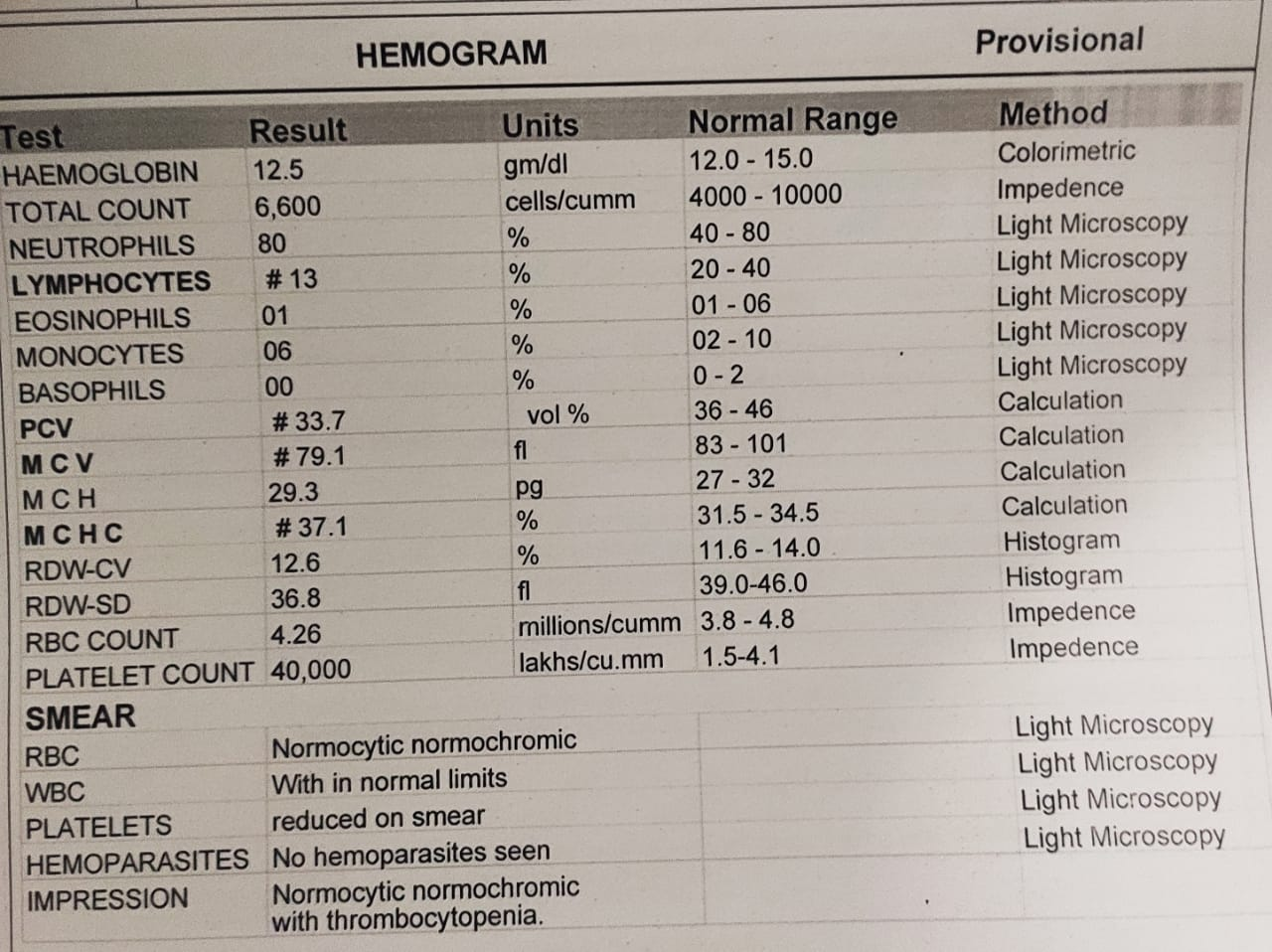
A 65 year old female patient came to casualty with complaints of Involuntary movements of tongue, involuntary micturition and defecation since 2 days. History of presenting illness: Patient was asymptomatic 1 month ago. Then, she developed involuntary movement of tongue. She had history of neck pain with back ache since 5 days. H/O vomitings since 2 days associated with nausea sensation, which was non bilious and non projectile. Past History: History of HTN AND DM present. General physical examination: Temp: afebrile PR 90/min RR 22 cpm BP 130/70mmHg SpO2 98% Systemic examination: CVS: S1 S2 + RS: BAE+, NVBS + CNS: Patient is conscious, slurred speech Motor examination: RIGHT LEFT Tone : UL incr ...