A YOUNG MALE REQUIRING GREAT EFFORT TO SQUAT..!!
Let me Introduce myself , I am G.ACHAL RAM currently in final year pursuing MBBS.
My aim of this section is to do a comprehensive assessment regarding the case provided by our interns.
The whole clinical data including history, clinical features and workup is provided in the below link.
https://hitesh116.blogspot.com/2020/05/12may-2020-elog-medicine-intern.html?m=1
After exploring the above case , the SUBJECTIVE COMPLAINTS are as follows :
Weakness of bilateral lower limbs since 20 days
Bilateral edema in lower limbs
H/O Difficulty in maintaining posture in squatting position and getting up from that position
H/O Difficulty in wearing and holding chappals.
On reviewing the chief complaints , focused assessment on CENTRAL NERVOUS SYSTEM , PERIPHERAL NERVOUS SYSTEM and MUSCULOSKELETAL SYSTEM must be on top priority to come up with a differential diagnosis and near possible provisional diagnosis.
DETAILED HISTORY OF PRESENT ILLNESS
WEAKNESS
Weakness initially started in the proximal region 2 years back , insidious in onset , progressed gradually to distal region , difficulty in wearing and holding chappals , difficulty in combing hair , buttoning and unbuttoning shirt.
B/L calf hypertrophy present.
NO SIGNIFICANT PAST HISTORY.
NO SIGNIFICANT FAMILY HISTORY.
NO SIGNIFICANT DRUG HISTORY.
GENERAL EXAMINATION-
-patient was conscious, coherent and cooperative.
-moderately built and nourished.
-no signs of pallor, icterus, clubbing, cyanosis , lymphadenopathy elicited.
- Bilateral calf hypertrophy noticed.
On Examination of vitals ,
Patient is afebrile , pulse rate found to be in normal range 92bpm .{NORMAL 60-100 bpm ] , breathing at rate of 18cycles/minute , recorded blood pressure 130/90 mm Hg , Saturation of oxygen found to be 96% and GRBS - 142mg/dl
LOCAL EXAMINATION
Patient is conscious, coherent, cooperative
Patient well oriented to time, place and person
Normal higher mental functions.
Cranial nerves- intact function.
Motor system-
Tone - normal
power - 4-/5 in both lower limbs
Reflexes absent in both lower limbs
Intact sensory system
No meningeal signs and cerebellar signs.
CVS EXAMINATION :
Palpable heart sound , palpable thrill in neck suggesting hyperdynamic circulation.
DIFFERENTIAL DIAGNOSIS :
Weakness is a common symptom with many causes which bears careful investigation.
IT IS IMPORTANT TO CLARIFY :
what the patient means—fatigue or actual loss of strength.
True motor weakness can arise from the CNS, a peripheral nerve, the neuromuscular junction, or a muscle.
Is the onset sudden, gradual or subacute, or chronic, over a long period of time?
What areas of the body are involved?
Is the weakness generalized, or focal to the face or a limb?
Does it involve one side of the body or both sides?
What movements are affected?
From the clinical data , we can infer most of the above questions.
Patient complaining of weakness in proximal regions since 2 years in the lower limbs , now gradually progressing to distal regions of limb, affecting both sides and movements like squatting, combing hair , wearing chappals and holding...are troubling her.
NOW THE MAIN QUERY ARISES THAT “ FROM WHICH ANATOMICAL REGION DOES THE WEAKNESS ARISES” ??
In evaluation of weakness ,
GOAL 1 : Whether it is myopathic or Neuropathic or Drug induced ?
LETS START EVALUATING NEUROLOGICAL CAUSE :
It is important to distinguish between UMN and LMN.
As UMN features like HYPERREFLEXIA , HYPERTONIA , SPASTIC PARALYSIS are not present in this patient , UMN is ruled out.
Lower motor neuron is defined as neuron that exit CNS and enter NMJ.
Lesion of LMN can be located at four places on its pathway
Anterior horn cell
Peripheral nerve
NMJ
Muscle (myopathy)
To rule out Anterior horn cell disease and peripheral neuropathy , evaluation of conduction velocity (NCV), histological findings , biochemical studies are necessary.
NCV testing has to be done in the patient , which helps us to know whether it is neurogenic.
ELECTROMYOGRAPHY is done and showing normal results , from which we can rule out NMJ disorders.
THE FOLLOWING HISTOPATHOLOGY REPORT CONFIRMS THAT PROBLEM WAS IN THE MUSCLE.( Muscle biopsy )
So now we can conclude that problem originating from muscle.
GOAL 2 : To detect what kind of etiology present in the muscle ,
Creating trouble to the patient.
GLUCOCORTICOID INDUCED MYOPATHY ? INFLAMMATORY MYOPATHIES ? HYPOTHYROID MYOPATHY ? STATIN INDUCED ?
GENETIC DISTURBANCES?
As patient is not known for any drug history , he is less likely for glucocorticoid induced myopathy and statin induced myopathy.
Normal thyroid status rules out hypothyroid myopathy (HOFFMAN’S DISEASE).
Chronic inflammatory demyelinating polyneuropathy is a diagnosis of exclusion and may present with relapsing-remitting events.
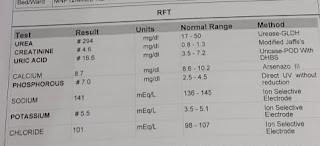
Renal function test done to rule out any muscle injury like rhabdomyolysis and the parameters turns out to be normal.
( RHABDOMYOLYSIS IS CONDITION IN WHICH DAMAGED SKELETAL MUSCLE BREAKS DOWN RAPIDLY AND PRESENTS WITH WEAKNESS ,MUSCLE PAIN , KIDNEY FAILURE )
Clinical presentation of B/L CALF HYPERTROPHY more likely to
Be Muscular dystrophy.
WHAT KIND OF MUSCULAR DYSTROPHY ?
DUCHENNE ? BECKER ? MYOTONIC ?
Can be differentiated and confirmed by genetic studies..
Most likely to be beckers muscular dystrophy because most of patients of DMD are wheelchair bound by adolescence ( here the patient is 18yr and walking with high stepping gait.)
MOST LIKELY DIAGNOSIS : BECKER’S MUSCULAR DYSTROPHY(X LINKED RECESSIVE)
Anatomical location causing weakness is most likely in muscle due to reduced Dystrophin .
(dystrophin is protein connecting cytoskeleton of muscle to extracellular membrane of muscle providing strength and stability to muscle )
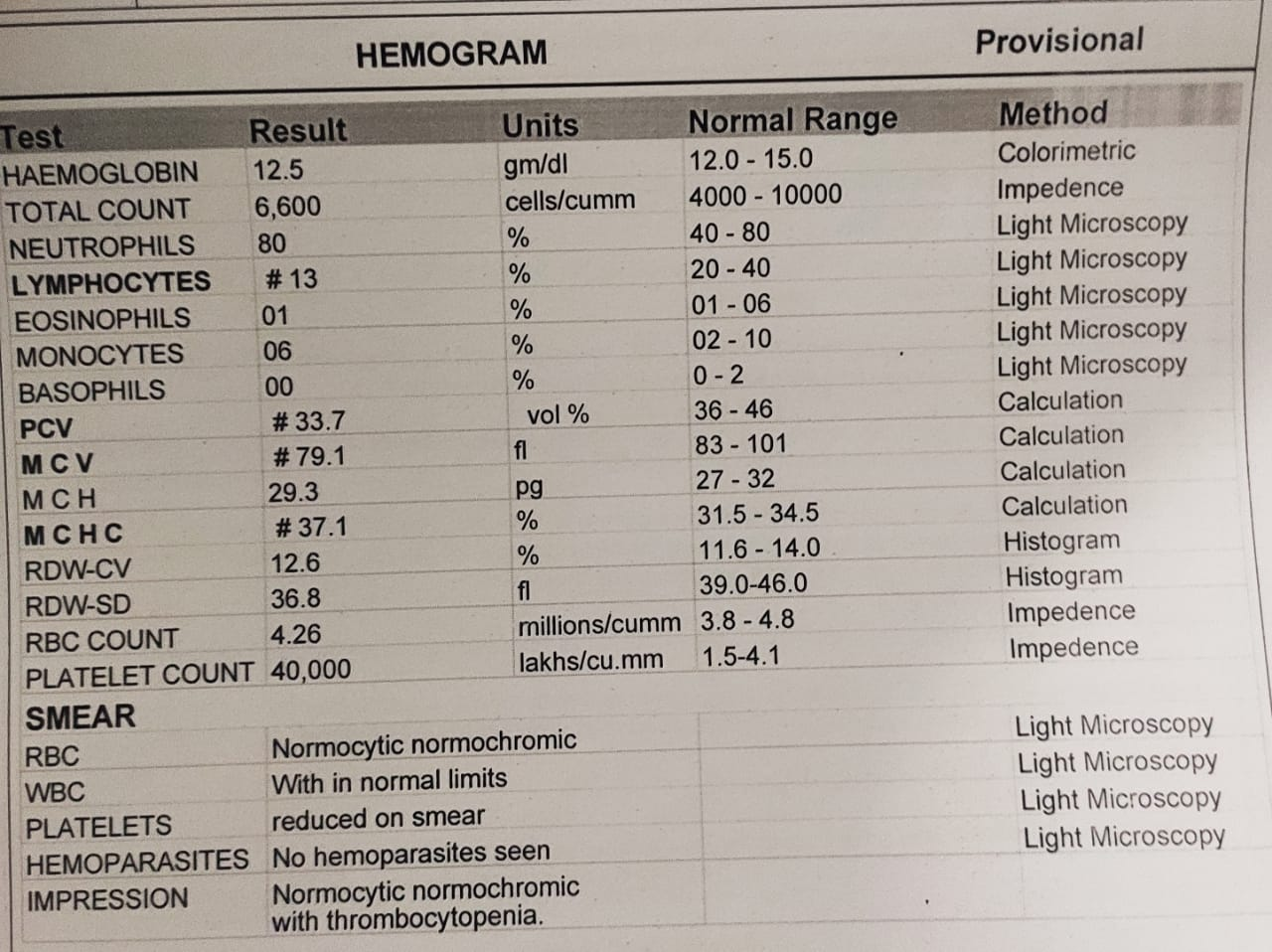
Biochemical abnormality : increased CK level (indicating some muscle damage )
IT PRESENTS WITH
Muscle weakness.
Use of Gower's maneuver to get up from floor
Pseudohypertrophy of calf muscles ( as muscle gets infiltrated with fat and connective tissue )
Heart muscle problems - cardiomyopathy
TREATMENT :
There is no known cure for Becker muscular dystrophy yet.
Inactivity or sitting down for too long can worsen the condition.
Physical therapy may be helpful to maintain muscle strength.
The drug prednisone contributes to an increased production of the protein utrophin which closely resembles dystrophin, the protein that is defective in BMD.(UTROPHIN BOOSTING)
Continuous monitoring of cardiac parameters is necessary , as the main cause of mortality is heart failure.
NEW STRATEGIES
Inserting new dystrophin genes
Using stem cells to repair damaged muscles.
Myostatin inhibition.
TREATMENT UNDERWENT IN HOSPITAL
T Prednisolone 15mg po od
T Pantop 40mg bbf
T Met xl 12.5mg od
Cap Becosules od
T Chymerol forte od - for treatment of pain and inflammation.
https://rarediseases.info.nih.gov/diseases/5900/becker-muscular-dystrophy
https://kidshealth.org/en/parents/becker-md.html

"THE FOLLOWING HISTOPATHOLOGY REPORT CONFIRMS THAT PROBLEM WAS IN THE MUSCLE.( Muscle biopsy )" but report show's No evidence found.
ReplyDeleteMy learning portfolio - http://classworkdecjan.blogspot.com/