21 year old male
This is an online e-log platform to discuss case scenarios of a patient with their guardian's permission.
I have been given this case to solve in an attempt to understand the topic of patient clinical data analysis to develop my competency in reading and comprehending clinical data including, history, clinical findings, investigations, and come up with a diagnosis and treatment plan.
A 21 year old male came to the OPD with complaints of
fever since one week.
abdominal pain and distention since one week.
loss of appetite since 1 week.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic one week ago then he developed fever which was High grade and intermittent and relieved on medication abdominal pain and distention since 1 week
-no history of vomiting , loose stools
-no history of headache
He got treated in a local hospital for 4 days for fever and he was referred to KIMS Narkatpally as his platelet count was low.
HISTORY OF PAST ILLNESS
Not a known case of Diabetes Mellitus, hypertension , Asthma , Epilepsy , Coronary artery disease , Tuberculosis.
PERSONAL HISTORY
Student by occupation who follows Mixed Diet, loss of appetite, regular bowel and bladder movements, no known addictions
FAMILY HISTORY:
His mother has Hypertension
GENERAL EXAMINATION
Patient is conscious , coherent and cooperative
Moderate build and not malnutri
His body temperature is 98.4 degree Farenheit
No pallor, icterus, cyanosis, clubbing, lymphadenopathy, pedal edema
SYSTEMIC EXAMINATION
Cardiovasular system: S1 and S2 are heard, No murmurs
Respiratory system: Bilateral air entry is present , Normal vesicular breath sounds are heard
Per Abdomen examination: soft nontender and bowel sounds present
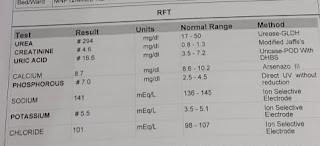
INVESTIGATIONS:
HEMOGRAM @17/08/21










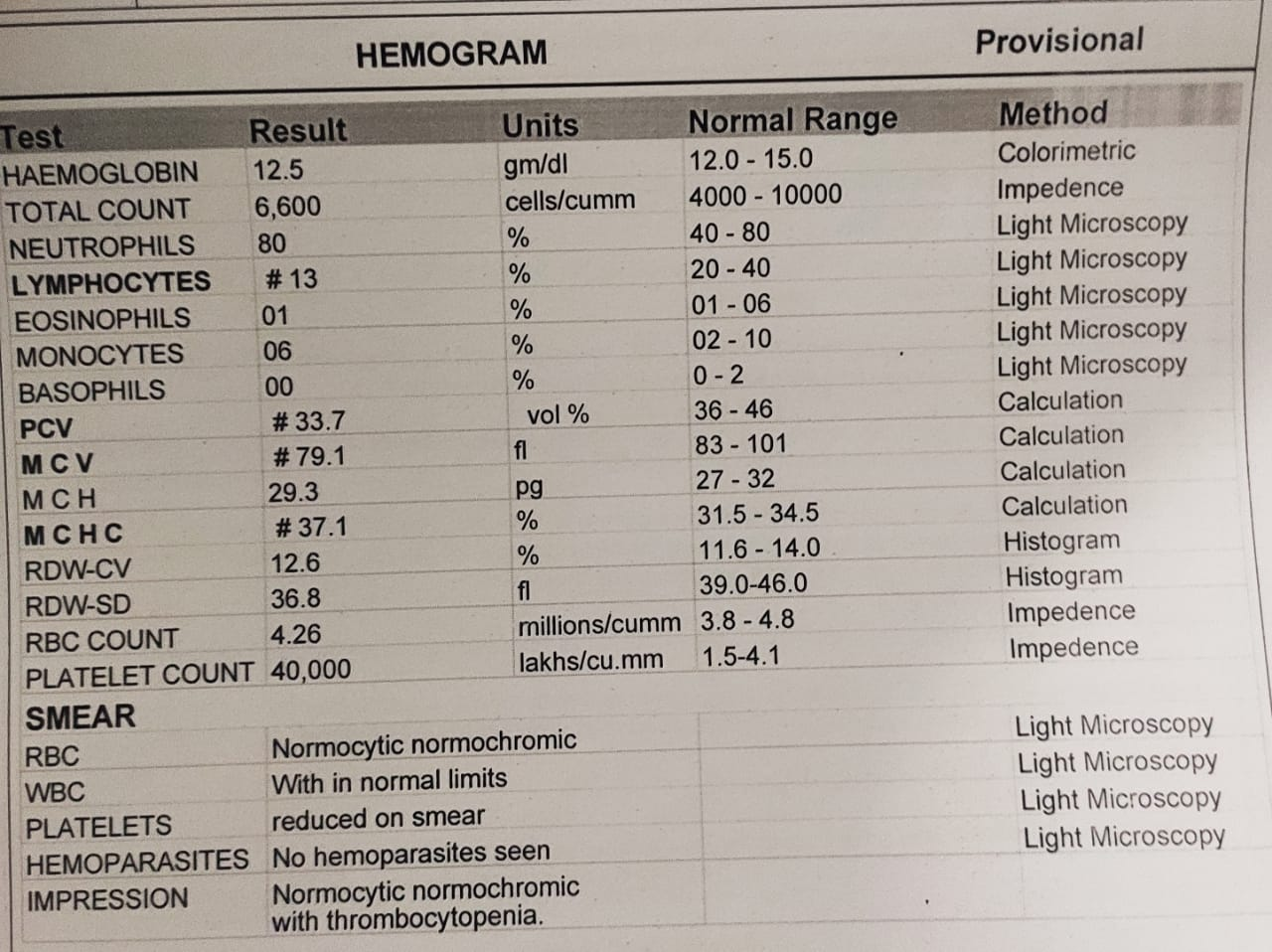
Comments
Post a Comment